All Posts
Dental Care Tips for Dementia Caregivers
Blende Dental Group
Dental care is one of the most challenging aspects of Alzheimer’s and dementia caregiving. Proper oral care is necessary to prevent eating difficulties, digestive problems and infections. As a caregiver, you may have to assist with dental hygiene or take a more hands-on approach. Below are helpful tips from professionals at the Blende Dental Group, which is home of the House Call Dentists, serving patients with special needs, including people with dementia.
Dr. David Blende a graduate of the University of Southern California and has more than 30 years of experience. He is also chief of dentistry at both California Pacific Medical Center and Kaiser Permanente’s San Francisco Medical Center, and on staff at six additional Bay Area hospitals.
Michelle Bernardo has been a Registered Dental Hygienist since 1994 when she graduated from New York University School of Dentistry. She divides her time between the Blende Dental Group San Francisco office and visiting homebound and elderly patients throughout the Bay Area.
Dr. Blende, you were one of the first dentists to perform house calls for patients. How did the idea about House Call Dentists come about?
When I first began my practice in Beverly Hills, I saw virtually no Alzheimer’s patients. When I started doing work in hospitals, I was called out to see home-bound people or patients for whom transport to the dental office was overwhelmingly difficult.
This fit into my background quite well. My father was a physician in a rural town close to the Canadian border and I used to go on house calls with him. Up until 1940, 47% of all interactions between a physician and a patient occurred in the home. And now physicians and medical groups are coming back around to that model.
Why is dental health critical to the health of people with Alzheimer’s?
There’s a huge taboo about being in the mouth of someone past a certain age and certainly in the mouth of our parents or spouse. 95% of all disease in the mouth is preventable. When we see patients who’ve had 35 years of good dentistry, we want to make sure that they hold on to that right to the very end.
A healthy mouth is one of the great privileges of health. Enjoying a meal is a great privilege of health. But because of these taboos about getting into a husband or a wife’s mouth, things go undiscovered. And when a problem is undiscovered, it becomes akin to abandoned because the patient ceases to brush their teeth regularly.
An abandoned mouth ultimately becomes a true nest of infection. The bacteria in the mouth overgrow and seed out into the heart, lungs and kidneys. We know now that one of the major causes of aspiration pneumonia are the bacteria that are harbored in between the teeth in an infected mouth. We also know that a lot of patients with late stage kidney disease have oral bacteria down in the kidneys.
We recommend that caregivers take their partners or parents who have Alzheimer’s to their regular dentist as soon as symptoms appear. Insist that the dentist clean up their mouth so that it can last the 7 to 10 years that are still before them.
Michelle, what are some warning signs that caregivers should watch out for to recognize when there might be a problem?
When a caregiver is taking care of a patient, what they want to look for immediately is an increase of plaque accumulation on the gum line. This is either due to dexterity issues or the person forgets to brush. Ultimately, this plaque accumulation would lead to tooth decay or gum infection. Another sign to watch out for would be if the person stops eating comfortably or you start to notice an unfinished plate at the end of the meal.
Do you have any prevention tips for caregivers?
Sure, as a caretaker you want to make sure you’re brushing the person’s teeth after every meal, ideally, but at least two times a day. Have the person rinse their teeth after snacks or after drinking juices. If the person has lost their ability to rinse, make sure you wipe the inside of their mouth with either a piece of gauze or wet wash cloth to get sugar and food particles off the teeth and cheeks. And then you’ll always want to be pulling the cheeks away from the teeth to see if there is anything broken or if there are any sores.
Dr. Blende, what do you advise the caregivers that you meet in your practice?
When we make house calls, the first thing we do is we ask the caregiver to show us their mouth. We want to know how well caregivers take care of their own mouth. That then becomes another part of the education. If they’re taking good care of their mouth, then we’re advancing down the line.
A great reminder for caregivers is to make sure that the person you are caring for has a good routine. It’s also important for the patient to be on a dental routine with their dentist, so make sure to have their mouth checked every few months. When someone has a toothache, it’s pretty simple to diagnose or if their face is swollen, that’s pretty simple, as well. But probably 85% of the insidious disease and the real infection is very silent and it slowly but perniciously starts to destroy the mouth so you have to get someone to look at it. Sometimes, I know, a client might have a headache because he takes a dose too high. You then should first refer him to a lower daily dose and see if he still has a headache. Other active molecules can also be tried, as they vary in the impact on an individual and may go through the body completely unnoticed when it comes to side effects. And finally, if falls short of his expectations, we have to discuss with a client all the means at our disposal: there are local creams, intracavernous injections and pumps.
Another problem is that as we age into 60’s, 70’s or 80’s, our saliva can diminish. When someone becomes distressed and they’re given anti-anxiety drugs or heart and pain medication, all of those have a side effect of drying out the mouth. And if the saliva dries, the mouth dries up. We like to tell people that saliva is like the tide at the beach. The tide comes up on the beach, picks up the kelp, makes it all wet, takes it into the ocean and puts it back on the beach. If someone, who’s been taking good care of their mouth for many years, begins taking one of the 400 drugs that causes dry mouth, you have a recipe for disaster.
What methods of treatment have you provided to individuals with dementia?
By the time we see an Alzheimer’s patient, they’ve been referred from their caregiver or from another dentist because they’ve fallen beyond the scope of that office’s ability to treat them. We gather the family together and individualize care. Some patients have had good care and some, unfortunately, are dealing with years of deferred maintenance and neglect. For these patients, we either offer palliative care, or if they want to restore the mouth so they can go back to enjoying food, we offer that option.
We treat patients either at our office with a physician anesthesiologist or in a hospital, depending on their health conditions. 70% of what we do is done under general anesthesia because by the time we see these patients, there’s a lot of catch-up treatment.
That’s the important point that I’d like to get across to families – if you can get their mouth stabilized before they go into the later stages of the disease, they’re way ahead of the curve. As the chief of a hospital division, before someone has to have radiation, they tell us to clean their mouth. Before chemotherapy, they ask us to clean up the mouth because they know what’s coming down the line. It should be the same way with Alzheimer’s. We know that there is a natural trajectory to the disease and what we want to do is make sure that oral disease is a non-issue in the late stages.
Helpful information related to this post:
Category
Archive
- April 7, 2025–April 13, 2025
- March 31, 2025–April 6, 2025
- March 24, 2025–March 30, 2025
- March 17, 2025–March 23, 2025
- March 10, 2025–March 16, 2025
- March 3, 2025–March 9, 2025
- February 24, 2025–March 2, 2025
- February 10, 2025–February 16, 2025
- February 3, 2025–February 9, 2025
- January 27, 2025–February 2, 2025
- January 20, 2025–January 26, 2025
- January 13, 2025–January 19, 2025
- December 16, 2024–December 22, 2024
- November 25, 2024–December 1, 2024
- August 26, 2024–September 1, 2024
- May 20, 2024–May 26, 2024
- April 22, 2024–April 28, 2024
- April 15, 2024–April 21, 2024
- April 8, 2024–April 14, 2024
- April 1, 2024–April 7, 2024
- March 25, 2024–March 31, 2024
- March 18, 2024–March 24, 2024
- March 11, 2024–March 17, 2024
- March 4, 2024–March 10, 2024
- February 26, 2024–March 3, 2024
- February 19, 2024–February 25, 2024
- February 12, 2024–February 18, 2024
- February 5, 2024–February 11, 2024
- January 29, 2024–February 4, 2024
- January 22, 2024–January 28, 2024
- January 15, 2024–January 21, 2024
- January 8, 2024–January 14, 2024
- December 4, 2023–December 10, 2023
- November 27, 2023–December 3, 2023
- November 6, 2023–November 12, 2023
- October 30, 2023–November 5, 2023
- October 23, 2023–October 29, 2023
- October 16, 2023–October 22, 2023
- October 9, 2023–October 15, 2023
- October 2, 2023–October 8, 2023
- September 25, 2023–October 1, 2023
- September 4, 2023–September 10, 2023
- December 19, 2022–December 25, 2022
- November 21, 2022–November 27, 2022
- October 24, 2022–October 30, 2022
- October 3, 2022–October 9, 2022
- August 22, 2022–August 28, 2022
- August 8, 2022–August 14, 2022
- August 1, 2022–August 7, 2022
- July 11, 2022–July 17, 2022
- July 4, 2022–July 10, 2022
- June 27, 2022–July 3, 2022
- June 20, 2022–June 26, 2022
- June 6, 2022–June 12, 2022
- May 23, 2022–May 29, 2022
- May 16, 2022–May 22, 2022
- May 9, 2022–May 15, 2022
- May 2, 2022–May 8, 2022
- April 25, 2022–May 1, 2022
- April 18, 2022–April 24, 2022
- April 11, 2022–April 17, 2022
- March 8, 2021–March 14, 2021
- December 14, 2020–December 20, 2020
- December 7, 2020–December 13, 2020
- July 6, 2020–July 12, 2020
- October 30, 2017–November 5, 2017
- September 18, 2017–September 24, 2017
- July 31, 2017–August 6, 2017
- May 1, 2017–May 7, 2017
- April 3, 2017–April 9, 2017
- February 6, 2017–February 12, 2017
- October 31, 2016–November 6, 2016
- December 17, 2012–December 23, 2012
- December 3, 2012–December 9, 2012
- November 26, 2012–December 2, 2012
- March 28, 2011–April 3, 2011
Related Articles
All Posts
How Artificial Intelligence Will Shape the Future Reality of Dentistry
Artificial Intelligence (AI) and Augmented Intelligence (AuI), once inhabitants of a realm relegated to science fiction, have become increasingly ubiquitous aspects of modern life. Every day, people tap into the…
bbadminist011
All Posts
This July 4, Let’s Focus on the Oral Health Needs of Patients Who Struggle with Independence
With the July 4 holiday right around the corner, the nation gathers to reflect on the nature of independence. Through fraught and bold decisions, the would-be founders of the United…
bbadminist011
All Posts
Bad Brushing Habits: Elbow Grease and Antiseptic Mouthwash Aren’t the Answer to Healthy Teeth
There’s an old joke that goes, “You brush your teeth at night to keep your teeth, you brush your teeth in the morning to keep your friends.” Humor aside, the…
bbadminist011
All Posts
June Is Oral Health Month: Time for a Shiny Summer Smile
Endorsed by the American Dental Association (ADA), Oral Health Month is a reminder about the importance of maintaining good oral hygiene. Every June, we celebrate the pioneering advances that have…
bbadminist011
All Posts
Proudly Display a Healthier Smile this LGBTQ+ Pride Month
June 1 marks the first day of LGBTQ+ Pride Month. Equality, inclusion, acceptance, and support for friends and loved ones in the community are critical to the advancement of our…
bbadminist011
All Posts
Over-the-Counter or Professional Teeth Whitening? For the Brightest Smile, See Your Dentist
Memorial Day is right around the corner, signaling the start of summer. It’s also the season when people return to wearing white. However, the quest for a brighter, whiter smile…
bbadminist011
All Posts
You May Be Surprised at How Your Dentist Can Help with Sleep Apnea
May is a month of many health awareness events, including sleep. Created by the Better Sleep Council (BSC), Better Sleep Month seeks to raise awareness about the benefits associated with…
bbadminist011
All Posts
Before Ordering Another Round, Know How Alcohol Affects Oral Health
Need a drink after a rough day? Is it “beer-thirty” yet? Are you meeting colleagues for an adult beverage at the local happy hour? Have you been to Napa and…
bbadminist011
All Posts
Asthma, Allergies, and Dental Problems: What You Need to Know
In 1984, the Asthma and Allergy Foundation of America (AAFA) declared the month of May to be “National Asthma and Allergy Awareness Month.” They chose this time of year because…
bbadminist011
All Posts
Yes, Kissing Can Cause Cavities, So Plan a Date with Your Dentist Before Your Tinder Match
All the kids are on TikTok, they say. TikTok has emerged as an immensely popular social network that relies on short-form user videos that span genres such as pranks, stunts,…
bbadminist011
All Posts
For Homebound Seniors, Consider the Gift of Oral Health for Mother’s Day
With Mother’s Day fast approaching, people around the country are preparing to pay tribute to the matriarchs of their families. Celebrations often include outings, gifts, flowers, cards, and meals at…
bbadminist011
All Posts
Braces or Clear Aligners? The Choice Involves More than Appearance
For many teens and adults, orthodontics offers a clear path toward straighter teeth and a more confident smile. Misaligned teeth are common and don’t generally pose oral health risks. So…
bbadminist011
All Posts
Everyone’s Stressed Out, and It’s a Real Pain in the…Mouth
We learned a lot during the past two years of dealing with a pandemic. For many people, one of those things was the word “bruxism.” Dentists around the country have…
bbadminist011
All Posts
It’s Time to See the Dentist and Overcome the Pandemic’s “Dental Disaster”
Health officials are warning of fresh COVID-19 outbreaks with new variants such as BA.2.12 and BA.2.12.1, surging across the United States. The fallout from the pandemic’s initial outbreak severely impacted…
bbadminist011
All Posts
How Teledentistry Is Removing Barriers to Dental Care
Until the pandemic, people never realized how much they would come to rely on virtual solutions. Digital communications have changed the way people communicate, shop, engage socially, and even manage…
bbadminist011
All Posts
April Is Here: That Means Flowers and National Facial Protection Month
Cities and states across the country have gradually lifted mask mandates that were imposed during the outbreak of COVID-19 and its variants. Generally speaking, no states are now directing people…
bbadminist011
All Posts
Looking for the Best Electric Toothbrush? Here Are Some Tips to Guide Your Decision
According to data from the Oral Health Foundation, 12 million Brits have switched to electric toothbrushes over the last five years. An estimated 34 million U.K. adults, 67% of the…
bbadminist011
All Posts
With Expanded Vaccinations and Safety Practices, There’s No Reason to Skip the Dentist
Prior to the pandemic, a disconcerting number of U.S. adults had routinely skipped visits to the dentist for basic care. Since the outbreak of COVID-19, those numbers have risen dramatically.…
Blende Dental Group
All Posts
COVID-19: What a Headache, What a Toothache
It’s probably not shocking news to most people that a resurgence of COVID-19 has come roaring back during the holiday season. Health officials warned early in the summer months that…
Blende Dental Group
All Posts
Preventative Care Is Essential to the Nation’s Homebound as COVID-19 Surges
The recent surge in coronavirus cases hasn’t just led to an alarming rise in hospitalizations and illness, it’s also forced officials in New York and California to reinstate shelter-in-place orders…
Blende Dental Group
All Posts
House call dental care for a homebound society
San Francisco/New York, May 6, 2020 — House Call Dentists announces the expansion and enhancement of its innovative dental care model to safely accommodate emergencies during this time of crisis.…
Blende Dental Group
All Posts
Activated Charcoal on Teeth – Is it Safe?
Activated charcoal is everywhere — from supplement pills to pressed juices to face masks. But is it safe to use on your teeth? Proponents say that brushing with activated charcoal…
Blende Dental Group
All Posts
What You Need to Know About Gum Care
There is no magic when it comes to maintaining the health of your gums. The key to a healthy smile is to make sure you are effectively removing the soft…
Blende Dental Group
All Posts
Patient Safety – What sets us apart?
The Blende Group and House Call Dentists have a unique expertise and service offering, which requires a unique set of skills. But we know skills and safety go hand in…
Blende Dental Group
All Posts
Xerostomia – The villain known as DRY MOUTH
by Blende Dental Group Seniors often suffer from Dry Mouth, which is a lack of sufficient saliva, making your mouth feel like a desert. However, Dry Mouth is not a…
Blende Dental Group
All Posts
Raising the bar: our standards for being a House Call Dentist
House call dentistry is a unique and highly specialized field. This requires providers that are properly vetted to take care of the vulnerable population they serve. In today’s blog we…
Blende Dental Group
All Posts
Resolutions Revisited – Diet trends and dental health
Happy New Year from the Blende Dental Group! 2017 is a new year, bringing with it a new opportunity to recommit to resolutions of health, like weight loss or adopting…
Blende Dental Group
All Posts
Recreational Cannabis and Oral Health
“Researchers have found that frequent recreational cannabis use – including marijuana, hashish, and hash oil – may be associated with elevated risk of periodontal (gum) disease.” The study recently published…
Blende Dental Group
All Posts
Sarah Marie
Sarah Marie is 90 years old and has dementia. Age Song’s memory care unit in San Francisco referred her to the practice. By performing a simple house call to her…
bbadminist011
All Posts
Fears and Phobias
Have you ever postponed or canceled a dental appointment because the thought of sitting in the dentist’s chair made you feel uncomfortable, nervous, or afraid? While sitting in the waiting…
bbadminist011
All Posts
Drug addiction & oral health
The Blende Dental Group focuses on treating patients with special needs, including those with chemical, or behavioral addictions. If you would like schedule an appointment or speak with a Patient…
bbadminist011
All Posts
Emergency Services FAQ
We offer the following emergency treatments: • Diagnosis & Treatment • Crowns, Bridges, Veneers • Extractions • Infections / Abscesses • Denture Adjustments • Root Canals • Pain Management Contact…
bbadminist011
All Posts
Patients with Head and Neck Cancer Need Comprehensive Dental Treatment
The Blende Dental Group focuses on treating patients with special needs, including those with head and neck cancer. Patients with head and neck cancer are often diagnosed in the later…
bbadminist011
Cancer
Oral Cancer Awareness Month: Time for a Spring Screening
More than 65% of working adults put off essential visits to the dentist. Their reasons vary. Some cite rigorous work schedules or family commitments that absorb much of their free…
bbadminist011
Dental Health
Value-Based Oral Health Care: Aligning with WHO’s Global Strategy on Oral Health
Oral health is an essential component of overall health and well-being. Value-based oral health care is the bridge between the mouth and the body. However, traditional dental care has often…
bbadminist011
Dental Health
World Oral Health Day 2025: How Oral Health Improves Mental Health
World Oral Health Day 2025, which falls on March 20, is a global initiative aimed at raising awareness about the critical importance of oral health and its profound impact on…
bbadminist011
Sedation Dentistry
Alzheimer’s Disease and Dentistry: Navigating Oral Health Challenges
Alzheimer’s disease is a progressive neurodegenerative disorder that primarily affects memory, cognitive function, and behavior. As the disease advances, patients face increasing challenges in managing their daily routines. That includes…
bbadminist011
Dental Health
The Oral Microbiome: How the Mouth Affects the Body and Why Value-Based Dentistry Is Key to Overall Health
There is an intricate relationship between oral and overall health. What goes on in your mouth can manifest into what happens in the rest of your body. The oral microbiome—a…
bbadminist011
Dental Health
Valentine’s Day and Your Oral Health: a Smile Worth Falling For
Valentine’s Day is all about love, romance, and probably a kiss or two. It’s a holiday when sweethearts and sweet treats come together. So this makes Valentine’s a great day…
bbadminist011
Dental Health
Climate Change Is Fueling Wildfires and Disasters; Sustainable Dentistry Can Make a Difference
The deadly California wildfires provide another stark reminder that the effects of climate change will continue to increase the prevalence of natural disasters across the country. The California Air Resources…
bbadminist011
All Posts
Celebrating a Season of Smiles: Happy Holidays from the Blende Dental Group
Happy holidays! As the winter holidays approach and 2024 draws to a close, we at the Blende Dental Group make sure to take time out from our routines to reflect…
bbadminist011
All Posts
Gratitude in Every Smile: A Thanksgiving Message from the Blende Dental Group
As the autumn leaves blanket the ground and the aroma of Thanksgiving feasts fills the air, we find ourselves reflecting on the many blessings that have graced our lives. This…
bbadminist011
Special Needs
Overcoming the Barriers to Accessible Dental Care for Disabled People
Disabled people, through their resilience and fortitude, have demonstrated throughout history their strength in overcoming obstacles. However, those challenges are more difficult to conquer when the barriers they face are…
bbadminist011
Special Needs
Autism Acceptance Month: The Importance of Oral Health Care for People with ASD
In recognition of Autism Acceptance Month, the Blende Dental Group is emphasizing the importance of oral health care for individuals with Autism Spectrum Disorder (ASD). They face unique challenges when…
bbadminist011
Dental Health
Hay Fever and Your Smile: The Link Between Allergies and Oral Health
Spring is in the air, and so too are the pollens that lead to hay fever. If you suffer from seasonal allergies, you’re well-acquainted with itchy eyes, sneezing fits, and…
bbadminist011
Dental Health
Menopause and Oral Health: The Link Between Hormonal Shifts and a Healthy Smile
For many women, menopause marks a significant shift in their physical and emotional wellbeing. Hot flashes, night sweats, and mood swings are often the first symptoms that come to mind.…
bbadminist011
Dental Health
Oral Health Literacy: Empowering Optimal Dental Outcomes
Oral health literacy is a growing area of focus in dentistry, and we at the Blende Dental Group are dedicated to empowering our patients with the knowledge they need to…
bbadminist011
Dental Health
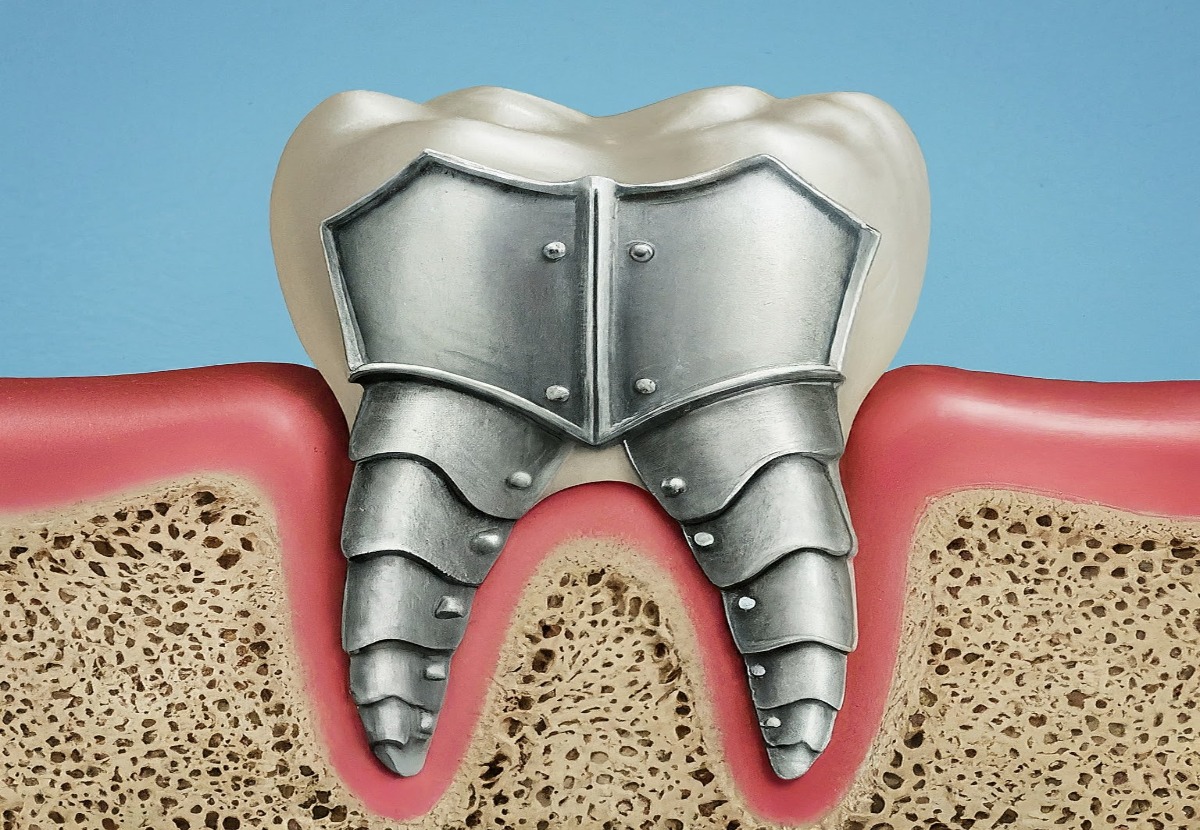
Understanding and Strengthening Weak Tooth Enamel for a Confident Smile
Tooth enamel is the armor that helps protect our teeth. However, not all enamel is created equally. Strong, healthy teeth are the foundation of a confident smile. They not only…
bbadminist011
Dental Health
New Bad Breath Research Unravels the Secrets of Halitosis and Potential Treatments
Bad breath, also known as halitosis, can be an embarrassing and socially isolating issue. However, the key to fresher breath may not simply be achieved by brushing and flossing more;…
bbadminist011
Special Needs
Smiles for All: Celebrating Children’s Dental Health Month with Special Needs in Mind
February is National Children's Dental Health Month, a time to focus on the importance of oral health for our little ones. However, for parents and caregivers of children with special…
bbadminist011
All Posts
Understanding TMJ Disorders: Shedding Light During TMJ Awareness Month
TMJ disorders are prevalent but not always fully comprehended. November is TMJ Awareness Month, a time when we come together to learn about this often misunderstood condition, its symptoms, causes,…
bbadminist011
All Posts
National Brush Day Celebrates the Toothbrush. But Just How Did the Most Famous Dental Device Come to Be?
With Halloween behind us and more holidays on the way, along with a bevy of sweets and treats, it’s no coincidence that National Brush Day is observed on November 1…
bbadminist011
Dental Health
Don’t Let Halloween Treats Become Oral Health Horror Stories
The bewitching season is upon us, and Halloween is lurking around the corner with its spooky charms and delightful confections. It’s a time when kids and adults revel in dressing…
bbadminist011
Dental Health
It’s National Seafood Month, Time to Explore the Oral Health Benefits of Seafood for Those Pearly Whites
This National Seafood Month, explore the incredible oral health benefits of seafood and how it can transform your smile. October is National Seafood Month, a time to celebrate the bountiful…
bbadminist011
Dental Health
Mental Health Issues Affect Oral Health, But Specialized Dental Care Is Available
Each year, millions of Americans face the reality of living with mental health issues, but because of persistent stigmas and the fear of discussing these conditions, too few people seek…
bbadminist011
Dental Health
The Future of Dentistry: Embracing Innovation and Personalization
The future of dentistry is defined by innovation in techniques and technologies, with an emphasis on personalization and comfort. For those concerned about their oral health, a brighter future and…
bbadminist011
All Posts
No White After Labor Day Shouldn’t Apply to Your Teeth: Here Are Some Tips for a Stunning Smile All Year
Outdated though the traditional may be, you could still face criticism from fashionistas for wearing white after Labor Day, a faux pas that invokes a throwback to the turn of…
bbadminist011
Dental Health
How Dentistry Has Changed to Support Patients in the New Normal of Digital, On Demand, Concierge Care
According to research from the Federal Reserve Bank of New York, Americans got back 60 million hours of their time as a result of remote work during the pandemic. So…
bbadminist011
All Posts
Happy Thanksgiving from the Blende Dental Group
Thanksgiving is tomorrow, and as we write this, families across the nation are preparing to gather in a celebration of the bonds that unite us. The spirit of this season…
bbadminist011
All Posts
You May Be Surprised to Learn that Dental House Calls Not Only Exist, They’re Thriving
House calls are firmly ingrained in the fabric of American culture and history. We’ve all heard stories about the country doctor who traveled across hill and dale to care for…
bbadminist011
All Posts
No Tricks, Just Tips for a Healthy Mouth this Halloween
With Halloween falling on a Monday this year, weekend gatherings and All Hallows Eve trick-or-treating mean costumed revelers may have three days’ worth of sweets and goodies to enjoy. That’s…
bbadminist011
All Posts
Virtual Reality Could Become a Real World Benefit to Dentists and Their Patients
With leaps in the development of Virtual Reality (VR), could dentistry become part of Mark Zuckerberg’s metaverse? VR is being used as an educational tool for students and as an…
bbadminist011
All Posts
Blende Dental Group Thrilled to Participate in the International Association for Disability and Oral Health Conference in Paris
From August 23 to 26, the 26th conference of the International Association for Disability and Oral Health (iADH) takes place in Paris. “The rights of vulnerable populations to achieve an…
bbadminist011
All Posts
Cigarettes, Vapes and Marijuana, Oh My: The Oral Health Risks of Smoking
The good news? Tobacco use has reached an historic low. The bad news? Vaping (using electronic cigarettes filled with juice or nicotine salt) and marijuana use are climbing. Vaping may…
bbadminist011
All Posts
The Cosmetic Dentistry Market Is Booming, Thanks to Technology and Technique
According to the July report “Cosmetic Dentistry Market Size, Share, Trends, By Product Type, By Patient Type, By End-Use, and By Region Forecast to 2028,” cosmetic dentistry is booming. Analysts…
bbadminist011
All Posts
People with Special Needs Are Facing a Growing But Seldom Discussed Oral Health Crisis
It requires little effort to peruse the daily news and uncover stories related to the growing health crisis in the country, whether the issues involve post-pandemic outbreaks, staffing shortages for…
bbadminist011
All Posts
How Artificial Intelligence Will Shape the Future Reality of Dentistry
Artificial Intelligence (AI) and Augmented Intelligence (AuI), once inhabitants of a realm relegated to science fiction, have become increasingly ubiquitous aspects of modern life. Every day, people tap into the…
bbadminist011
All Posts
This July 4, Let’s Focus on the Oral Health Needs of Patients Who Struggle with Independence
With the July 4 holiday right around the corner, the nation gathers to reflect on the nature of independence. Through fraught and bold decisions, the would-be founders of the United…
bbadminist011
All Posts
Bad Brushing Habits: Elbow Grease and Antiseptic Mouthwash Aren’t the Answer to Healthy Teeth
There’s an old joke that goes, “You brush your teeth at night to keep your teeth, you brush your teeth in the morning to keep your friends.” Humor aside, the…
bbadminist011
All Posts
June Is Oral Health Month: Time for a Shiny Summer Smile
Endorsed by the American Dental Association (ADA), Oral Health Month is a reminder about the importance of maintaining good oral hygiene. Every June, we celebrate the pioneering advances that have…
bbadminist011
All Posts
Proudly Display a Healthier Smile this LGBTQ+ Pride Month
June 1 marks the first day of LGBTQ+ Pride Month. Equality, inclusion, acceptance, and support for friends and loved ones in the community are critical to the advancement of our…
bbadminist011
All Posts
Over-the-Counter or Professional Teeth Whitening? For the Brightest Smile, See Your Dentist
Memorial Day is right around the corner, signaling the start of summer. It’s also the season when people return to wearing white. However, the quest for a brighter, whiter smile…
bbadminist011
All Posts
You May Be Surprised at How Your Dentist Can Help with Sleep Apnea
May is a month of many health awareness events, including sleep. Created by the Better Sleep Council (BSC), Better Sleep Month seeks to raise awareness about the benefits associated with…
bbadminist011
All Posts
Before Ordering Another Round, Know How Alcohol Affects Oral Health
Need a drink after a rough day? Is it “beer-thirty” yet? Are you meeting colleagues for an adult beverage at the local happy hour? Have you been to Napa and…
bbadminist011
All Posts
Asthma, Allergies, and Dental Problems: What You Need to Know
In 1984, the Asthma and Allergy Foundation of America (AAFA) declared the month of May to be “National Asthma and Allergy Awareness Month.” They chose this time of year because…
bbadminist011
All Posts
Yes, Kissing Can Cause Cavities, So Plan a Date with Your Dentist Before Your Tinder Match
All the kids are on TikTok, they say. TikTok has emerged as an immensely popular social network that relies on short-form user videos that span genres such as pranks, stunts,…
bbadminist011
All Posts
For Homebound Seniors, Consider the Gift of Oral Health for Mother’s Day
With Mother’s Day fast approaching, people around the country are preparing to pay tribute to the matriarchs of their families. Celebrations often include outings, gifts, flowers, cards, and meals at…
bbadminist011
All Posts
Braces or Clear Aligners? The Choice Involves More than Appearance
For many teens and adults, orthodontics offers a clear path toward straighter teeth and a more confident smile. Misaligned teeth are common and don’t generally pose oral health risks. So…
bbadminist011
All Posts
Everyone’s Stressed Out, and It’s a Real Pain in the…Mouth
We learned a lot during the past two years of dealing with a pandemic. For many people, one of those things was the word “bruxism.” Dentists around the country have…
bbadminist011
All Posts
It’s Time to See the Dentist and Overcome the Pandemic’s “Dental Disaster”
Health officials are warning of fresh COVID-19 outbreaks with new variants such as BA.2.12 and BA.2.12.1, surging across the United States. The fallout from the pandemic’s initial outbreak severely impacted…
bbadminist011
All Posts
How Teledentistry Is Removing Barriers to Dental Care
Until the pandemic, people never realized how much they would come to rely on virtual solutions. Digital communications have changed the way people communicate, shop, engage socially, and even manage…
bbadminist011
All Posts
April Is Here: That Means Flowers and National Facial Protection Month
Cities and states across the country have gradually lifted mask mandates that were imposed during the outbreak of COVID-19 and its variants. Generally speaking, no states are now directing people…
bbadminist011
All Posts
Looking for the Best Electric Toothbrush? Here Are Some Tips to Guide Your Decision
According to data from the Oral Health Foundation, 12 million Brits have switched to electric toothbrushes over the last five years. An estimated 34 million U.K. adults, 67% of the…
bbadminist011
All Posts
With Expanded Vaccinations and Safety Practices, There’s No Reason to Skip the Dentist
Prior to the pandemic, a disconcerting number of U.S. adults had routinely skipped visits to the dentist for basic care. Since the outbreak of COVID-19, those numbers have risen dramatically.…
Blende Dental Group
All Posts
COVID-19: What a Headache, What a Toothache
It’s probably not shocking news to most people that a resurgence of COVID-19 has come roaring back during the holiday season. Health officials warned early in the summer months that…
Blende Dental Group
All Posts
Preventative Care Is Essential to the Nation’s Homebound as COVID-19 Surges
The recent surge in coronavirus cases hasn’t just led to an alarming rise in hospitalizations and illness, it’s also forced officials in New York and California to reinstate shelter-in-place orders…
Blende Dental Group
All Posts
House call dental care for a homebound society
San Francisco/New York, May 6, 2020 — House Call Dentists announces the expansion and enhancement of its innovative dental care model to safely accommodate emergencies during this time of crisis.…
Blende Dental Group
All Posts
Activated Charcoal on Teeth – Is it Safe?
Activated charcoal is everywhere — from supplement pills to pressed juices to face masks. But is it safe to use on your teeth? Proponents say that brushing with activated charcoal…
Blende Dental Group
All Posts
What You Need to Know About Gum Care
There is no magic when it comes to maintaining the health of your gums. The key to a healthy smile is to make sure you are effectively removing the soft…
Blende Dental Group
All Posts
Patient Safety – What sets us apart?
The Blende Group and House Call Dentists have a unique expertise and service offering, which requires a unique set of skills. But we know skills and safety go hand in…
Blende Dental Group
All Posts
Xerostomia – The villain known as DRY MOUTH
by Blende Dental Group Seniors often suffer from Dry Mouth, which is a lack of sufficient saliva, making your mouth feel like a desert. However, Dry Mouth is not a…
Blende Dental Group
All Posts
Raising the bar: our standards for being a House Call Dentist
House call dentistry is a unique and highly specialized field. This requires providers that are properly vetted to take care of the vulnerable population they serve. In today’s blog we…
Blende Dental Group
All Posts
Resolutions Revisited – Diet trends and dental health
Happy New Year from the Blende Dental Group! 2017 is a new year, bringing with it a new opportunity to recommit to resolutions of health, like weight loss or adopting…
Blende Dental Group
All Posts
Recreational Cannabis and Oral Health
“Researchers have found that frequent recreational cannabis use – including marijuana, hashish, and hash oil – may be associated with elevated risk of periodontal (gum) disease.” The study recently published…
Blende Dental Group
All Posts
Sarah Marie
Sarah Marie is 90 years old and has dementia. Age Song’s memory care unit in San Francisco referred her to the practice. By performing a simple house call to her…
bbadminist011
All Posts
Fears and Phobias
Have you ever postponed or canceled a dental appointment because the thought of sitting in the dentist’s chair made you feel uncomfortable, nervous, or afraid? While sitting in the waiting…
bbadminist011
All Posts
Drug addiction & oral health
The Blende Dental Group focuses on treating patients with special needs, including those with chemical, or behavioral addictions. If you would like schedule an appointment or speak with a Patient…
bbadminist011
All Posts
Emergency Services FAQ
We offer the following emergency treatments: • Diagnosis & Treatment • Crowns, Bridges, Veneers • Extractions • Infections / Abscesses • Denture Adjustments • Root Canals • Pain Management Contact…
bbadminist011
All Posts
Patients with Head and Neck Cancer Need Comprehensive Dental Treatment
The Blende Dental Group focuses on treating patients with special needs, including those with head and neck cancer. Patients with head and neck cancer are often diagnosed in the later…
bbadminist011
Cancer
Oral Cancer Awareness Month: Time for a Spring Screening
More than 65% of working adults put off essential visits to the dentist. Their reasons vary. Some cite rigorous work schedules or family commitments that absorb much of their free…
bbadminist011
Dental Health
Value-Based Oral Health Care: Aligning with WHO’s Global Strategy on Oral Health
Oral health is an essential component of overall health and well-being. Value-based oral health care is the bridge between the mouth and the body. However, traditional dental care has often…
bbadminist011
Dental Health
World Oral Health Day 2025: How Oral Health Improves Mental Health
World Oral Health Day 2025, which falls on March 20, is a global initiative aimed at raising awareness about the critical importance of oral health and its profound impact on…
bbadminist011
Sedation Dentistry
Alzheimer’s Disease and Dentistry: Navigating Oral Health Challenges
Alzheimer’s disease is a progressive neurodegenerative disorder that primarily affects memory, cognitive function, and behavior. As the disease advances, patients face increasing challenges in managing their daily routines. That includes…
bbadminist011
Dental Health
The Oral Microbiome: How the Mouth Affects the Body and Why Value-Based Dentistry Is Key to Overall Health
There is an intricate relationship between oral and overall health. What goes on in your mouth can manifest into what happens in the rest of your body. The oral microbiome—a…
bbadminist011
Dental Health
Valentine’s Day and Your Oral Health: a Smile Worth Falling For
Valentine’s Day is all about love, romance, and probably a kiss or two. It’s a holiday when sweethearts and sweet treats come together. So this makes Valentine’s a great day…
bbadminist011
Dental Health
Climate Change Is Fueling Wildfires and Disasters; Sustainable Dentistry Can Make a Difference
The deadly California wildfires provide another stark reminder that the effects of climate change will continue to increase the prevalence of natural disasters across the country. The California Air Resources…
bbadminist011
All Posts
Celebrating a Season of Smiles: Happy Holidays from the Blende Dental Group
Happy holidays! As the winter holidays approach and 2024 draws to a close, we at the Blende Dental Group make sure to take time out from our routines to reflect…
bbadminist011
All Posts
Gratitude in Every Smile: A Thanksgiving Message from the Blende Dental Group
As the autumn leaves blanket the ground and the aroma of Thanksgiving feasts fills the air, we find ourselves reflecting on the many blessings that have graced our lives. This…
bbadminist011
Special Needs
Overcoming the Barriers to Accessible Dental Care for Disabled People
Disabled people, through their resilience and fortitude, have demonstrated throughout history their strength in overcoming obstacles. However, those challenges are more difficult to conquer when the barriers they face are…
bbadminist011
Special Needs
Autism Acceptance Month: The Importance of Oral Health Care for People with ASD
In recognition of Autism Acceptance Month, the Blende Dental Group is emphasizing the importance of oral health care for individuals with Autism Spectrum Disorder (ASD). They face unique challenges when…
bbadminist011
Dental Health
Hay Fever and Your Smile: The Link Between Allergies and Oral Health
Spring is in the air, and so too are the pollens that lead to hay fever. If you suffer from seasonal allergies, you’re well-acquainted with itchy eyes, sneezing fits, and…
bbadminist011
Dental Health
Menopause and Oral Health: The Link Between Hormonal Shifts and a Healthy Smile
For many women, menopause marks a significant shift in their physical and emotional wellbeing. Hot flashes, night sweats, and mood swings are often the first symptoms that come to mind.…
bbadminist011
Dental Health
Oral Health Literacy: Empowering Optimal Dental Outcomes
Oral health literacy is a growing area of focus in dentistry, and we at the Blende Dental Group are dedicated to empowering our patients with the knowledge they need to…
bbadminist011
Dental Health
Understanding and Strengthening Weak Tooth Enamel for a Confident Smile
Tooth enamel is the armor that helps protect our teeth. However, not all enamel is created equally. Strong, healthy teeth are the foundation of a confident smile. They not only…
bbadminist011
Dental Health
New Bad Breath Research Unravels the Secrets of Halitosis and Potential Treatments
Bad breath, also known as halitosis, can be an embarrassing and socially isolating issue. However, the key to fresher breath may not simply be achieved by brushing and flossing more;…
bbadminist011
Special Needs
Smiles for All: Celebrating Children’s Dental Health Month with Special Needs in Mind
February is National Children's Dental Health Month, a time to focus on the importance of oral health for our little ones. However, for parents and caregivers of children with special…
bbadminist011
All Posts
Understanding TMJ Disorders: Shedding Light During TMJ Awareness Month
TMJ disorders are prevalent but not always fully comprehended. November is TMJ Awareness Month, a time when we come together to learn about this often misunderstood condition, its symptoms, causes,…
bbadminist011
All Posts
National Brush Day Celebrates the Toothbrush. But Just How Did the Most Famous Dental Device Come to Be?
With Halloween behind us and more holidays on the way, along with a bevy of sweets and treats, it’s no coincidence that National Brush Day is observed on November 1…
bbadminist011
Dental Health
Don’t Let Halloween Treats Become Oral Health Horror Stories
The bewitching season is upon us, and Halloween is lurking around the corner with its spooky charms and delightful confections. It’s a time when kids and adults revel in dressing…
bbadminist011
Dental Health
It’s National Seafood Month, Time to Explore the Oral Health Benefits of Seafood for Those Pearly Whites
This National Seafood Month, explore the incredible oral health benefits of seafood and how it can transform your smile. October is National Seafood Month, a time to celebrate the bountiful…
bbadminist011
Dental Health
Mental Health Issues Affect Oral Health, But Specialized Dental Care Is Available
Each year, millions of Americans face the reality of living with mental health issues, but because of persistent stigmas and the fear of discussing these conditions, too few people seek…
bbadminist011
Dental Health
The Future of Dentistry: Embracing Innovation and Personalization
The future of dentistry is defined by innovation in techniques and technologies, with an emphasis on personalization and comfort. For those concerned about their oral health, a brighter future and…
bbadminist011
All Posts
No White After Labor Day Shouldn’t Apply to Your Teeth: Here Are Some Tips for a Stunning Smile All Year
Outdated though the traditional may be, you could still face criticism from fashionistas for wearing white after Labor Day, a faux pas that invokes a throwback to the turn of…
bbadminist011
Dental Health
How Dentistry Has Changed to Support Patients in the New Normal of Digital, On Demand, Concierge Care
According to research from the Federal Reserve Bank of New York, Americans got back 60 million hours of their time as a result of remote work during the pandemic. So…
bbadminist011
All Posts
Happy Thanksgiving from the Blende Dental Group
Thanksgiving is tomorrow, and as we write this, families across the nation are preparing to gather in a celebration of the bonds that unite us. The spirit of this season…
bbadminist011
All Posts
You May Be Surprised to Learn that Dental House Calls Not Only Exist, They’re Thriving
House calls are firmly ingrained in the fabric of American culture and history. We’ve all heard stories about the country doctor who traveled across hill and dale to care for…
bbadminist011
All Posts
No Tricks, Just Tips for a Healthy Mouth this Halloween
With Halloween falling on a Monday this year, weekend gatherings and All Hallows Eve trick-or-treating mean costumed revelers may have three days’ worth of sweets and goodies to enjoy. That’s…
bbadminist011
All Posts
Virtual Reality Could Become a Real World Benefit to Dentists and Their Patients
With leaps in the development of Virtual Reality (VR), could dentistry become part of Mark Zuckerberg’s metaverse? VR is being used as an educational tool for students and as an…
bbadminist011
All Posts
Blende Dental Group Thrilled to Participate in the International Association for Disability and Oral Health Conference in Paris
From August 23 to 26, the 26th conference of the International Association for Disability and Oral Health (iADH) takes place in Paris. “The rights of vulnerable populations to achieve an…
bbadminist011
All Posts
Cigarettes, Vapes and Marijuana, Oh My: The Oral Health Risks of Smoking
The good news? Tobacco use has reached an historic low. The bad news? Vaping (using electronic cigarettes filled with juice or nicotine salt) and marijuana use are climbing. Vaping may…
bbadminist011
All Posts
The Cosmetic Dentistry Market Is Booming, Thanks to Technology and Technique
According to the July report “Cosmetic Dentistry Market Size, Share, Trends, By Product Type, By Patient Type, By End-Use, and By Region Forecast to 2028,” cosmetic dentistry is booming. Analysts…
bbadminist011
All Posts
People with Special Needs Are Facing a Growing But Seldom Discussed Oral Health Crisis
It requires little effort to peruse the daily news and uncover stories related to the growing health crisis in the country, whether the issues involve post-pandemic outbreaks, staffing shortages for…
bbadminist011
Let's brighten
that smile
The when and where are up to you.